We Must Tackle Antimicrobial Resistance Before Its Too Late
We must tackle antimicrobial resistance before its too late – We Must Tackle Antimicrobial Resistance Before It’s Too Late – a stark warning that echoes across the globe. The rise of antimicrobial resistance (AMR) is a silent pandemic, threatening to unravel the very foundations of modern medicine. From everyday infections to complex surgeries, the effectiveness of antibiotics is being eroded, leaving us vulnerable to a world where simple infections can once again become deadly.
Imagine a world where a simple cut could lead to a life-threatening infection, where routine surgeries become high-risk procedures, and where common illnesses like pneumonia could once again become fatal. This is the chilling reality we face if we don’t act now to combat antimicrobial resistance.
This crisis is not a distant threat; it’s happening right now, impacting hospitals, farms, and our environment.
The Urgency of Antimicrobial Resistance: We Must Tackle Antimicrobial Resistance Before Its Too Late
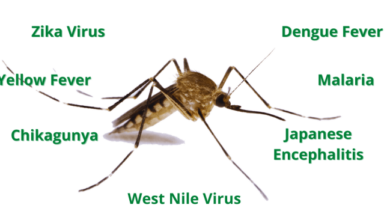
Antimicrobial resistance (AMR) is a growing global health crisis that threatens to undo decades of progress in medicine and public health. It occurs when bacteria, viruses, fungi, and parasites develop resistance to antimicrobial drugs, making infections harder to treat and increasing the risk of death.
This resistance is a natural phenomenon, but it is being accelerated by the overuse and misuse of antibiotics.
The Current State of Antimicrobial Resistance Globally
AMR is a global problem, affecting every country in the world. According to the World Health Organization (WHO), antimicrobial resistance is a major threat to global health security. The WHO estimates that by 2050, antimicrobial resistance could cause 10 million deaths annually and cost the global economy $100 trillion.
It’s easy to get caught up in the drama of fictional worlds, like the shocking revelation that robin officially kills batgirl in DC’s most brutal world. But while these stories are captivating, we can’t forget about the real-world challenges we face, like the urgent need to tackle antimicrobial resistance.
This silent threat could undo all the progress we’ve made in medicine, so we must act now before it’s too late.
The Potential Consequences of Unchecked Resistance
Unchecked antimicrobial resistance could have devastating consequences for individuals, communities, and the global economy.
We can’t afford to be complacent about antimicrobial resistance – it’s a silent threat that could undo decades of medical progress. Just like we need to be prepared for the impact of extreme weather events, like the heavy rain expected to bring flooding and travel disruption , we need to act now to combat this growing crisis.
The consequences of inaction are simply too dire to ignore.
- Increased mortality rates:Infections that were once easily treatable with antibiotics could become deadly, leading to a surge in deaths from preventable diseases.
- Longer hospital stays and higher healthcare costs:Patients with resistant infections require longer hospital stays and more intensive care, which drives up healthcare costs.
- Economic disruptions:The rise of AMR could lead to disruptions in agricultural production, food security, and global trade, as resistant pathogens spread to animals and crops.
Antimicrobial Resistance Impacts Healthcare, Agriculture, and the Environment, We must tackle antimicrobial resistance before its too late
The consequences of AMR extend beyond healthcare, impacting agriculture and the environment.
The threat of antimicrobial resistance looms large, and we must act now to prevent a future where even simple infections become deadly. It’s a crisis that demands global attention, especially as Europe careens toward a downturn as its biggest economies fight crises at home , diverting resources and focus.
We can’t afford to let this silent killer gain ground; our health and the future of our societies depend on a united front against antimicrobial resistance.
Healthcare
- Infections become more difficult to treat:Resistant bacteria can spread easily in healthcare settings, leading to outbreaks of difficult-to-treat infections.
- Increased use of expensive and toxic drugs:When common antibiotics fail, doctors may have to resort to using more expensive and toxic drugs, which can have serious side effects.
- Surgeries and transplants become riskier:AMR makes surgeries and transplants riskier, as patients are more susceptible to infections.
Agriculture
- Reduced food production:Resistant bacteria can infect livestock and crops, leading to reduced yields and economic losses.
- Increased use of antibiotics in animals:The overuse of antibiotics in animal agriculture contributes to the spread of AMR.
- Food safety concerns:Resistant bacteria can contaminate food, posing a risk to human health.
Environment
- Spread of resistant bacteria:Resistant bacteria can spread through the environment, contaminating water, soil, and air.
- Impact on ecosystems:Resistant bacteria can harm beneficial microorganisms in the environment, disrupting ecological balance.
- Potential for new and emerging threats:The spread of AMR could lead to the emergence of new and dangerous pathogens.
The Root Causes of Antimicrobial Resistance
Antimicrobial resistance (AMR) is a complex global health threat, and its emergence and spread are driven by a multitude of factors. Understanding the root causes is crucial for developing effective strategies to combat this growing crisis.
Overuse and Misuse of Antibiotics
Antibiotics are powerful medications that target and kill bacteria, but their overuse and misuse contribute significantly to the development of AMR. When antibiotics are used unnecessarily or inappropriately, bacteria are exposed to these drugs, creating selective pressure that favors the survival and multiplication of resistant strains.
- Prescription Practices:In some settings, antibiotics are prescribed too readily for conditions that don’t require them, such as viral infections, where they are ineffective. This practice creates a breeding ground for resistance.
- Self-medication:Individuals sometimes purchase antibiotics over-the-counter or use leftover prescriptions without consulting a doctor, leading to inappropriate use and the emergence of resistant strains.
- Agricultural Use:Antibiotics are widely used in animal agriculture to promote growth and prevent disease. This practice exposes bacteria to sub-therapeutic doses of antibiotics, contributing to the development of resistance genes that can spread to humans through the food chain.
Poor Infection Control Practices and Sanitation
Effective infection control measures are essential for preventing the spread of infections and reducing the emergence of AMR. However, inadequate hygiene practices, poor sanitation, and insufficient infection control measures in healthcare settings and communities can facilitate the transmission of resistant bacteria.
- Healthcare-Associated Infections:Hospitals and other healthcare facilities are often hotspots for the transmission of resistant bacteria. Inadequate hand hygiene, improper disinfection of equipment, and lack of isolation procedures for infected patients can contribute to the spread of AMR.
- Community Transmission:Poor sanitation and hygiene in communities can also facilitate the spread of resistant bacteria. Inadequate access to clean water, poor waste management, and crowded living conditions create environments where resistant bacteria can thrive and spread.
Strategies for Combating Antimicrobial Resistance
Antimicrobial resistance (AMR) poses a significant threat to global health, food security, and economic development. To effectively address this growing crisis, we must implement a comprehensive and multi-faceted approach that targets the root causes of resistance and promotes responsible use of antimicrobials across all sectors.
This involves a combination of strategies aimed at reducing the emergence and spread of resistance, optimizing antimicrobial use, and developing new treatments and diagnostic tools.
A Comprehensive Plan for Tackling Antimicrobial Resistance
A comprehensive plan for tackling antimicrobial resistance should address multiple levels of intervention, including individual behavior, healthcare systems, agricultural practices, and environmental factors.
- Public awareness and education: Raising public awareness about AMR and promoting responsible use of antibiotics is crucial. This can be achieved through educational campaigns, public health initiatives, and community engagement programs.
- Surveillance and monitoring: Robust surveillance systems are essential to track the emergence and spread of resistant organisms, allowing for early detection and timely intervention.
- Research and development: Investing in research and development of new antibiotics, vaccines, and diagnostic tools is crucial to combat resistance and develop alternative treatment strategies.
- International collaboration: Addressing AMR requires global cooperation and coordinated efforts to share knowledge, resources, and best practices.
- Policy and regulation: Strong policies and regulations are needed to govern the use of antimicrobials in human and animal health, agriculture, and the environment.
Best Practices for Antibiotic Stewardship in Healthcare Settings
Antibiotic stewardship programs aim to optimize antibiotic use in healthcare settings, minimizing unnecessary prescriptions and promoting appropriate treatment regimens.
- Restricting antibiotic use: Limiting the use of antibiotics for non-bacterial infections, such as viral infections, can help prevent the emergence of resistance.
- Promoting appropriate prescribing: Educating healthcare providers about appropriate antibiotic selection, dosage, and duration of treatment is essential to minimize unnecessary use.
- Infection prevention and control: Implementing robust infection prevention and control measures, such as hand hygiene, can reduce the spread of infections and the need for antibiotics.
- Monitoring and evaluation: Regularly monitoring antibiotic use and resistance patterns allows for continuous improvement and adaptation of stewardship programs.
Strategies for Preventing Resistance in Agriculture and the Environment
Antimicrobial use in agriculture contributes to the emergence and spread of resistance. Therefore, strategies to minimize antimicrobial use in agriculture and the environment are crucial.
- Reducing antimicrobial use in livestock production: Implementing alternative strategies, such as vaccination, biosecurity measures, and improved animal husbandry practices, can reduce the reliance on antibiotics.
- Restricting the use of antibiotics for growth promotion: Using antibiotics solely for therapeutic purposes, rather than for growth promotion, can significantly reduce overall antibiotic use.
- Promoting responsible use of antimicrobials in aquaculture: Similar strategies to those used in livestock production can be applied to aquaculture to reduce antimicrobial use and prevent resistance.
- Minimizing antibiotic contamination of the environment: Implementing wastewater treatment and proper disposal of animal waste can reduce the spread of resistant bacteria into the environment.
Public Awareness and Education
The fight against antimicrobial resistance (AMR) requires a multifaceted approach, and public awareness and education play a crucial role in this battle. By empowering individuals with knowledge about AMR and promoting responsible antibiotic use, we can significantly reduce the spread of resistant bacteria and safeguard public health.
Public Awareness Campaigns
Effective public awareness campaigns can educate individuals about AMR and its implications. These campaigns should aim to raise awareness about the following:* The nature of AMR:AMR occurs when bacteria evolve and become resistant to antibiotics, making infections harder to treat.
The consequences of AMR
Untreated infections can lead to prolonged illness, increased healthcare costs, and even death.
The role of antibiotics
Antibiotics are essential for treating bacterial infections, but they are not effective against viral infections like the common cold.
The importance of responsible antibiotic use
Misusing antibiotics can contribute to AMR.
- Targeted messaging:Campaigns should be tailored to specific audiences, such as healthcare professionals, patients, and the general public. For example, a campaign aimed at healthcare professionals might emphasize the importance of prescribing antibiotics only when necessary and following appropriate guidelines.
- Use of various media:Public awareness campaigns can leverage a variety of media platforms, including television, radio, social media, and print publications. Engaging visuals, compelling narratives, and relatable examples can enhance campaign effectiveness.
- Community engagement:Involving community leaders, health organizations, and local stakeholders can broaden the reach and impact of public awareness campaigns. Community-based initiatives can provide tailored information and support to specific populations.
Promoting Responsible Antibiotic Use
Effective communication strategies can promote responsible antibiotic use, reducing the risk of AMR. Here are some key strategies:
- Educate individuals about the proper use of antibiotics:Emphasize that antibiotics are only effective against bacterial infections and should not be used to treat viral infections.
- Encourage individuals to complete the full course of antibiotics as prescribed:Stopping antibiotics early can lead to the development of resistant bacteria.
- Promote self-care measures for common viral infections:Encourage individuals to rely on rest, fluids, and over-the-counter medications to manage common illnesses like the cold and flu.
- Highlight the importance of preventative measures:Emphasize the role of vaccination, hand hygiene, and other infection prevention practices in reducing the need for antibiotics.
Personal Hygiene and Infection Prevention
Maintaining good personal hygiene and practicing effective infection prevention measures are essential in combating AMR. These practices help to reduce the spread of bacteria and the development of resistance.
- Frequent handwashing:Washing hands frequently with soap and water, especially after using the restroom, before eating, and after contact with sick individuals, can significantly reduce the spread of bacteria.
- Proper cough etiquette:Covering the mouth and nose when coughing or sneezing with a tissue or elbow can prevent the spread of germs.
- Safe food handling:Properly cooking food, washing hands before handling food, and storing food at appropriate temperatures can minimize the risk of foodborne illnesses.
- Vaccination:Vaccinations protect against a range of infectious diseases, reducing the need for antibiotics.
- Avoiding unnecessary contact with healthcare settings:Limiting exposure to healthcare settings, especially when healthy, can reduce the risk of acquiring antibiotic-resistant bacteria.
Global Collaboration and Policy
Antimicrobial resistance is a global health crisis that demands a collaborative and coordinated approach. No single country or organization can effectively address this challenge alone. International cooperation is crucial to developing and implementing effective strategies to combat resistance and ensure access to essential antimicrobial medicines for all.
International Cooperation and Policy Initiatives
International collaboration is essential for tackling antimicrobial resistance. It enables the sharing of knowledge, resources, and best practices, fostering a global response to this multifaceted challenge. Several key policy initiatives and regulations have been established to guide and coordinate global efforts in combating resistance.
- The World Health Organization (WHO) has played a pivotal role in raising awareness and promoting action against antimicrobial resistance. WHO has developed a Global Action Plan on Antimicrobial Resistance, outlining a comprehensive strategy for addressing the issue. This plan encourages countries to implement national action plans, promote responsible antimicrobial use, and invest in research and development of new antimicrobial drugs.
- The United Nations General Assembly has recognized antimicrobial resistance as a serious threat to global health and development. In 2016, the General Assembly adopted a resolution calling for a coordinated global response to antimicrobial resistance, urging countries to strengthen their national action plans and collaborate on research, surveillance, and education.
- The Global Antibiotic Research and Development Partnership (GARDP) is a non-profit organization dedicated to developing new antibiotics and other antimicrobials to address the growing threat of resistance. GARDP works with pharmaceutical companies, research institutions, and governments to accelerate the development and availability of effective antimicrobials.
Role of Governments, Healthcare Organizations, and Pharmaceutical Companies
Governments, healthcare organizations, and pharmaceutical companies all play critical roles in combating antimicrobial resistance.
- Governmentshave a responsibility to implement policies that promote responsible antimicrobial use, strengthen surveillance systems, and invest in research and development of new antimicrobials. Governments can also support public awareness campaigns to educate the public about the importance of antimicrobial stewardship.
- Healthcare organizationsplay a vital role in ensuring appropriate antimicrobial use in clinical settings. Hospitals and clinics should implement antimicrobial stewardship programs to monitor antimicrobial use, optimize prescribing practices, and promote infection prevention and control measures.
- Pharmaceutical companiesare responsible for developing new antimicrobials and ensuring their availability. They also have a role in promoting responsible antimicrobial use and supporting research into new approaches to combat resistance.