We Cant Let Monkeypox Repeat COVID-19
We cant let monkeypox turn into a repeat of covid – We Can’t Let Monkeypox Repeat COVID-19. That’s a stark reality we must confront. The world is still reeling from the COVID-19 pandemic, and the emergence of monkeypox presents a chilling reminder of the fragility of our health systems and the interconnectedness of our global community.
The potential for this virus to become another widespread pandemic is very real, and we must act decisively to prevent that from happening.
Monkeypox, like COVID-19, is a zoonotic disease, meaning it can spread from animals to humans. The virus can also spread from person to person through close contact, including direct contact with an infected person’s rash, respiratory droplets, and contaminated materials.
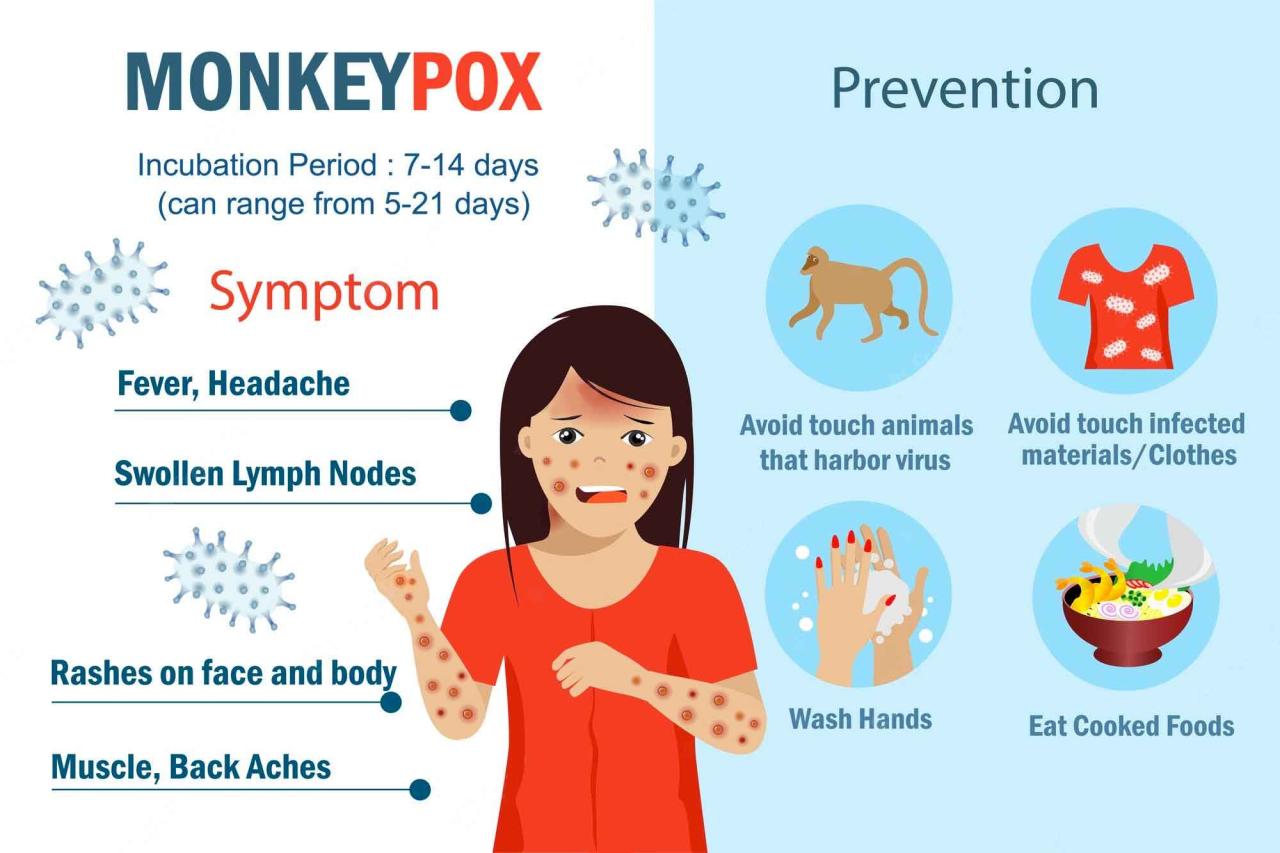
The symptoms of monkeypox can include fever, headache, muscle aches, swollen lymph nodes, and a rash that can look like pimples or blisters. While monkeypox is typically less severe than COVID-19, it can still be a serious illness, especially for those with weakened immune systems.
The potential for long-term health complications from monkeypox is also unknown.
The Urgency of Prevention

The recent emergence of monkeypox has sparked concerns about its potential to become a global pandemic, similar to COVID-19. While monkeypox is not as easily transmissible as COVID-19, its ability to spread through close contact and potentially through respiratory droplets necessitates immediate and decisive action to prevent a widespread outbreak.
We can’t let monkeypox turn into a repeat of COVID, with misinformation and panic fueling the fire. It’s crucial to rely on accurate information from experts like Dr. Henning Tiemeier, whose insightful perspectives on the outbreak can be found in the transcript of his recent interview.
By understanding the facts and taking necessary precautions, we can prevent monkeypox from becoming a widespread crisis.
The Potential Consequences of a Monkeypox Pandemic
A monkeypox pandemic could have significant consequences for public health, economies, and social systems.
We can’t let monkeypox turn into a repeat of COVID, and that means focusing on proactive measures, like increased awareness and access to vaccines. It’s also important to remember that strong leadership is crucial in navigating these kinds of public health crises, as we’ve seen with the recent appointment of Santa Ono as the new president of the University of Michigan following the ouster of Mark Schlissel.
By learning from past mistakes and prioritizing responsible action, we can hopefully avoid another pandemic-like scenario.
- Overwhelmed Healthcare Systems:A surge in monkeypox cases could overwhelm healthcare systems, leading to delays in treatment and potential shortages of essential resources like vaccines and antiviral medications.
- Economic Disruptions:Similar to COVID-19, a monkeypox pandemic could disrupt economic activity, leading to business closures, supply chain disruptions, and job losses.
- Social and Psychological Impacts:The fear and uncertainty associated with a pandemic can lead to social isolation, mental health issues, and increased stigma towards affected individuals and communities.
The Importance of Early Intervention
History has shown that early intervention and proactive measures are crucial in preventing the spread of infectious diseases.
- The 1918 Spanish Flu Pandemic:The delayed response to the 1918 Spanish flu pandemic, coupled with inadequate public health measures, resulted in millions of deaths worldwide.
- The Ebola Outbreak in West Africa:The Ebola outbreak in West Africa in 2014 highlighted the importance of early detection, isolation, and contact tracing in controlling an outbreak.
Understanding Monkeypox
Monkeypox is a viral disease that has been making headlines recently, and it’s important to understand its nature and potential impact. This disease, caused by the monkeypox virus, has been around for decades, but its recent resurgence has raised concerns about its potential to become a global health threat.
The news of Michael Stenger, the ousted Senate Sergeant at Arms, passing away at 71 is a reminder that life is precious and fleeting. It’s a stark contrast to the global concern over monkeypox, which we must not allow to become another COVID-19 scenario.
We need to act swiftly and decisively to prevent the spread of this virus, just as we learned from the tragic events that led to Stenger’s removal from his post, as detailed in this article: michael stenger ousted senate sergeant at arms dies at 71.
We can’t afford to be complacent; the consequences of inaction could be devastating.
Origins and Transmission
The monkeypox virus is a member of the orthopoxvirus genus, which also includes the variola virus that causes smallpox. While the exact origins of the virus are still being investigated, it is believed to have originated in Africa, where it is endemic in certain animal populations.
The virus can be transmitted from animals to humans through direct contact with infected animals, their blood, or bodily fluids. Human-to-human transmission can occur through close contact with an infected person, including through respiratory droplets, skin lesions, or contaminated materials.
Symptoms of Monkeypox, We cant let monkeypox turn into a repeat of covid
Monkeypox typically presents with flu-like symptoms, such as fever, headache, muscle aches, and swollen lymph nodes. A characteristic rash develops a few days after the onset of these symptoms, starting as flat, red lesions that eventually become raised and filled with fluid.
These lesions can appear on the face, hands, feet, and other parts of the body.
Comparing Monkeypox and COVID-19
While both monkeypox and COVID-19 are viral diseases, there are significant differences between them. COVID-19 is caused by a coronavirus, while monkeypox is caused by an orthopoxvirus. The transmission routes of these viruses also differ. COVID-19 primarily spreads through respiratory droplets, while monkeypox can spread through close contact with infected individuals or contaminated materials.
| Feature | Monkeypox | COVID-19 |
|---|---|---|
| Cause | Monkeypox virus (orthopoxvirus) | SARS-CoV-2 (coronavirus) |
| Transmission | Close contact with infected individuals, contaminated materials, or infected animals | Respiratory droplets, aerosols |
| Symptoms | Fever, headache, muscle aches, swollen lymph nodes, rash | Fever, cough, shortness of breath, fatigue, loss of taste or smell |
| Severity | Generally mild, but can be severe in some cases | Can range from mild to severe, with potential for complications |
| Treatment | Supportive care, antiviral medications | Antiviral medications, supportive care, monoclonal antibodies |
Global Situation and Hotspots
Monkeypox has been reported in several countries outside of Africa, including Europe, North America, and Australia. This recent spread has raised concerns about the potential for a global outbreak. The World Health Organization (WHO) has declared the monkeypox outbreak a public health emergency of international concern, highlighting the need for coordinated global efforts to contain its spread.
“The current monkeypox outbreak is a significant public health concern, requiring a coordinated global response to prevent further spread and protect vulnerable populations.”
WHO
Current hotspots for monkeypox cases include:
- Europe: Spain, Portugal, Germany, France, and the United Kingdom have reported a significant number of cases.
- North America: The United States, Canada, and Mexico have also seen a rise in monkeypox cases.
- Africa: Cases continue to be reported in several African countries, where the virus is endemic.
Lessons Learned from COVID-19
The COVID-19 pandemic was a global crisis that exposed vulnerabilities in our public health systems and highlighted the need for improved preparedness for future outbreaks. As we face the emergence of monkeypox, it is crucial to learn from the mistakes made during the COVID-19 pandemic and implement strategies to prevent a similar scenario.
The Importance of Effective Communication
Effective communication is paramount in managing outbreaks. During the COVID-19 pandemic, inconsistent messaging, conflicting information, and a lack of transparency from authorities contributed to public confusion and distrust. This led to the spread of misinformation and hampered efforts to control the virus.
- Public health officials must communicate clearly, consistently, and transparently with the public about the risks, symptoms, and preventive measures associated with the disease.
- Information should be tailored to different audiences, taking into account cultural and linguistic diversity.
- Utilizing multiple communication channels, including traditional media, social media, and community outreach programs, can help reach a wider audience.
The Role of Public Trust in Shaping the Response to Infectious Diseases
Public trust is essential for effective disease control. When people trust public health authorities, they are more likely to follow guidelines, seek testing and treatment, and participate in vaccination programs. However, during the COVID-19 pandemic, trust in public health institutions eroded due to factors such as inconsistent messaging, misinformation, and political interference.
- Building and maintaining public trust requires transparency, accountability, and ethical decision-making.
- Engaging with communities and addressing concerns openly can foster trust and encourage collaboration.
- Public health officials must be mindful of the impact of their communication on public trust and strive to provide accurate and reliable information.
Strengthening Public Health Infrastructure
The COVID-19 pandemic exposed weaknesses in public health infrastructure, including inadequate testing capacity, insufficient contact tracing resources, and a shortage of healthcare workers. These deficiencies hindered efforts to contain the virus and exacerbated its impact.
- Investing in robust public health infrastructure, including surveillance systems, laboratory capacity, and trained personnel, is crucial for early detection and response to outbreaks.
- Developing a readily deployable workforce of public health professionals, including epidemiologists, contact tracers, and community health workers, is essential for effective outbreak management.
- Strengthening partnerships between public health agencies, healthcare providers, and community organizations can enhance coordination and ensure a comprehensive response.
The Importance of International Collaboration
Infectious diseases do not respect borders, and effective outbreak management requires international collaboration. During the COVID-19 pandemic, the lack of coordinated global response, including delays in sharing information and resources, contributed to the rapid spread of the virus.
- International collaboration is essential for sharing data, expertise, and resources to combat infectious diseases.
- Establishing robust mechanisms for rapid information sharing and coordinated response among countries is crucial for preventing outbreaks from becoming pandemics.
- Supporting global health initiatives, such as the World Health Organization (WHO), can strengthen international collaboration and enhance preparedness for future outbreaks.
Outcome Summary: We Cant Let Monkeypox Turn Into A Repeat Of Covid
We must learn from the mistakes of the past and act swiftly and decisively to prevent monkeypox from becoming a widespread pandemic. We need to increase awareness, improve public health infrastructure, and strengthen international collaboration. By working together, we can mitigate the risks of monkeypox and protect ourselves and our communities.






