NY Group Homes Scrutinized After Nursing Home COVID Crisis
Covid cases in new york group homes under scrutiny after nursing home controversy – The COVID-19 pandemic exposed vulnerabilities in long-term care facilities, with New York’s nursing homes becoming the focal point of a national controversy. Now, the spotlight is shifting to group homes, raising questions about their preparedness and the potential for similar outbreaks.
While nursing homes were initially the target of public scrutiny, concerns are growing about the potential for widespread COVID-19 transmission in group homes, which often house individuals with disabilities or mental health conditions.
These facilities, often smaller and less equipped than nursing homes, face unique challenges in managing COVID-19. Residents may have underlying health conditions that make them more susceptible to the virus, and staff may lack the training or resources to implement robust infection control measures.
The lack of adequate testing, staffing shortages, and limited access to personal protective equipment (PPE) are just some of the hurdles that group homes face, mirroring the struggles experienced by nursing homes during the pandemic’s early stages.
The New York Nursing Home Controversy
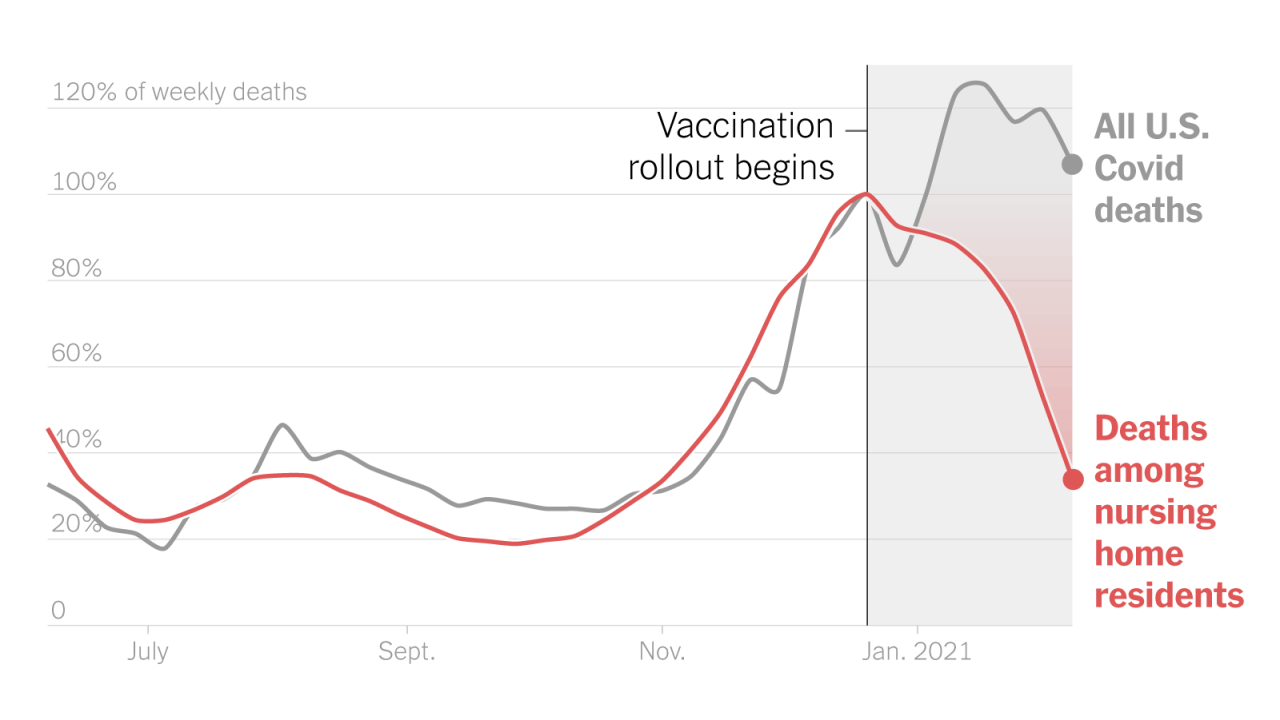
The New York nursing home controversy erupted in the early days of the COVID-19 pandemic, focusing on the state’s policies regarding the admission of COVID-19 positive patients into nursing homes. This policy, implemented in March 2020, became a subject of intense scrutiny and criticism, leading to investigations and lawsuits.
The Policy and Its Rationale
On March 25, 2020, New York State issued a directive that prohibited nursing homes from denying admission or readmission to residents based solely on a positive COVID-19 test result. The rationale behind this policy was to prevent hospitals from being overwhelmed with patients and to ensure that individuals in need of long-term care had access to appropriate facilities.
The scrutiny of COVID-19 cases in New York group homes, following the nursing home controversy, highlights the ongoing challenges of protecting vulnerable populations. This focus on health and safety comes at a time when consumer spending patterns are shifting, with a recent epic goods buying spree wanes as consumers ramp up services spending.
This shift suggests a growing desire for experiences and services, potentially impacting the allocation of resources for long-term care facilities like group homes, which are crucial in ensuring the well-being of those most at risk.
This policy was intended to alleviate pressure on hospitals and ensure continuity of care for residents. However, it sparked a heated debate and raised concerns about the potential risks to vulnerable populations in nursing homes.
Public Outcry and Criticism
The policy drew immediate criticism from various quarters, including families of nursing home residents, healthcare professionals, and elected officials. Critics argued that the policy put nursing home residents at a higher risk of contracting COVID-19, particularly given the high vulnerability of this population to the virus.
They expressed concern that the policy would lead to a surge in infections and deaths in nursing homes. The policy faced strong opposition from families who feared for the safety of their loved ones in nursing homes.
Investigations and Lawsuits
The controversy led to investigations by the New York State Attorney General’s Office, the U.S. Department of Justice, and the New York State Legislature. These investigations focused on the state’s policies, the number of COVID-19 cases and deaths in nursing homes, and the adequacy of the state’s response to the pandemic.
Additionally, several lawsuits were filed against the state government, alleging negligence and misconduct in handling the pandemic in nursing homes.
Group Homes Under Scrutiny
The controversy surrounding COVID-19 outbreaks in New York nursing homes has cast a spotlight on the vulnerability of other congregate living settings, including group homes. These facilities, which provide housing and support services for individuals with disabilities, are now facing increased scrutiny regarding their preparedness and response to the pandemic.
The Connection Between Nursing Homes and Group Homes
The concerns about group homes stem directly from the lessons learned during the nursing home crisis. Both types of facilities share common characteristics that make them susceptible to COVID-19 outbreaks:
High population density
Group homes, like nursing homes, often house multiple individuals in close proximity, increasing the risk of transmission.
Vulnerable populations
Residents of both types of facilities are often older or have underlying health conditions, making them more susceptible to severe illness from COVID-19.
Limited resources
Group homes, particularly smaller facilities, may have fewer staff and resources to implement robust infection control measures.
Concerns Regarding COVID-19 Cases in Group Homes
Several specific concerns have been raised regarding COVID-19 cases in group homes:
Lack of transparency
There is a lack of comprehensive data on COVID-19 cases in group homes, making it difficult to assess the extent of the problem.
Inadequate testing and screening
Some group homes have faced challenges in providing timely and widespread testing for residents and staff, potentially leading to undetected cases.
Staff shortages
Like nursing homes, group homes have struggled with staff shortages, which can impact their ability to provide adequate care and implement infection control measures.
Limited access to personal protective equipment (PPE)
Some group homes have reported difficulties obtaining sufficient PPE for staff and residents, further increasing the risk of transmission.
The scrutiny of COVID cases in New York group homes, following the nursing home controversy, brings to mind the recent news of a retired general being investigated for undisclosed lobbying for Qatar, a story that highlights the potential for conflicts of interest in government and private sectors.
Both situations raise questions about transparency and accountability, especially when it comes to vulnerable populations like those residing in group homes and nursing facilities.
Potential Vulnerabilities of Group Homes to COVID-19 Outbreaks
Group homes face several vulnerabilities that contribute to their susceptibility to COVID-19 outbreaks:
Limited space
Group homes may have limited space to isolate residents who test positive for COVID-19, increasing the risk of spreading the virus to other residents.
Shared living spaces
The recent scrutiny of COVID cases in New York group homes, following the controversy surrounding nursing homes, highlights a crucial issue: the politicization of public health. It’s reminiscent of how influential election deniers, who often push conspiracy theories and misinformation, have fueled a fight to control elections, as explored in this insightful article.
This pattern of distrust and manipulation, unfortunately, has become a dangerous trend, impacting both our healthcare system and our democratic processes. The situation with group homes underscores the need for transparent, evidence-based decision-making, free from political agendas.
Residents in group homes often share common areas like kitchens, dining rooms, and bathrooms, making it difficult to maintain physical distancing.
Staff interaction
Group home staff often have close contact with residents, increasing their risk of exposure to the virus and potentially transmitting it to others.
Resident mobility
Some residents may have mobility limitations or require assistance with activities of daily living, making it challenging to implement strict infection control measures.
Challenges Faced by Group Homes and Nursing Homes in Managing COVID-19
Both group homes and nursing homes face similar challenges in managing COVID-19:
Staffing shortages
Both types of facilities have experienced significant staff shortages due to illness, quarantine requirements, and burnout, making it difficult to provide adequate care.
Access to testing and PPE
Both group homes and nursing homes have faced challenges in obtaining timely and adequate testing and PPE, particularly during periods of high demand.
Financial strain
Both types of facilities have experienced financial strain due to increased costs associated with COVID-19, such as testing, PPE, and staffing.
Communication challenges
Both group homes and nursing homes have faced challenges in communicating effectively with residents, families, and staff about COVID-19 protocols and updates.
Impact on Residents and Staff: Covid Cases In New York Group Homes Under Scrutiny After Nursing Home Controversy
The COVID-19 pandemic had a profound impact on residents and staff in group homes across New York State. Outbreaks of the virus in these facilities resulted in significant health challenges, emotional distress, and disruption of daily routines.
Impact on Residents
The COVID-19 pandemic posed significant health risks to residents of group homes, particularly those with underlying health conditions. The virus spread rapidly in congregate settings, leading to outbreaks that resulted in serious illness and even death. The impact on residents included:
- Increased risk of infection: Group homes are high-risk environments due to close proximity and shared living spaces, making residents more susceptible to contracting the virus.
- Severe illness and hospitalization: Residents with underlying health conditions, such as respiratory illnesses or compromised immune systems, were at higher risk of experiencing severe COVID-19 symptoms requiring hospitalization.
- Social isolation and loneliness: Restrictions on visitation and group activities to prevent the spread of the virus led to isolation and loneliness among residents, impacting their mental and emotional well-being.
- Disruption of routine and care: The pandemic disrupted daily routines, including access to therapy, recreational activities, and other essential services, affecting their overall quality of life.
Impact on Staff, Covid cases in new york group homes under scrutiny after nursing home controversy
Staff members working in group homes faced immense challenges during the pandemic, including:
- Increased workload: Staff shortages and the need for additional safety measures, such as increased cleaning and sanitation, led to increased workloads and stress.
- Risk of infection: Staff members were at risk of contracting the virus themselves, particularly while caring for residents with COVID-19.
- Emotional distress: Witnessing residents struggle with illness and the impact of isolation on their mental health took an emotional toll on staff members.
- Lack of support: Staff members often faced limited access to personal protective equipment (PPE), training, and mental health support services, further adding to their stress and anxiety.
Challenges in Accessing Healthcare and Support Services
Both residents and staff faced challenges in accessing healthcare and support services during the pandemic:
- Limited access to healthcare: Restrictions on visitors and concerns about the spread of the virus made it difficult for residents to access routine medical care and specialists.
- Disruptions in mental health services: The pandemic disrupted mental health services, leading to delays in therapy appointments and limited access to support groups for residents and staff.
- Limited access to testing and treatment: Delays in testing and treatment availability made it difficult to identify and manage cases effectively, particularly in the early stages of the pandemic.
- Lack of resources: Group homes often lacked sufficient resources, including PPE, cleaning supplies, and staff, to adequately address the needs of residents during the pandemic.
Psychological and Emotional Toll
The pandemic had a profound psychological and emotional impact on residents and staff:
- Increased anxiety and stress: The constant threat of infection, social isolation, and uncertainty about the future led to heightened anxiety and stress for residents and staff.
- Depression and grief: The loss of loved ones, the disruption of daily routines, and the inability to participate in social activities contributed to depression and grief among residents and staff.
- Trauma: The experience of illness, isolation, and the loss of loved ones can be traumatic for residents and staff, leading to long-term emotional and psychological consequences.
- Fear and uncertainty: The pandemic created a sense of fear and uncertainty about the future, making it difficult for residents and staff to plan for the future and feel secure.
Final Review
The pandemic has forced a critical examination of long-term care practices, highlighting the need for enhanced safety measures and increased resources to protect vulnerable populations. As we move forward, it’s imperative to learn from the mistakes made in nursing homes and ensure that group homes are equipped to prevent and manage COVID-19 outbreaks.
This includes investing in training for staff, providing adequate PPE, and implementing robust infection control protocols. By addressing these challenges, we can work towards a future where all residents in long-term care settings have access to safe and supportive environments.