Medicare Advantage Plans Often Deny Needed Care, Federal Report Finds
Medicare advantage plans often deny needed care federal report finds – Medicare Advantage Plans Often Deny Needed Care, Federal Report Finds, a recent report from the federal government has revealed a concerning trend: Medicare Advantage plans are frequently denying necessary care to their beneficiaries. This finding has sparked widespread concern, as it raises questions about the quality and accessibility of healthcare for millions of Americans.
The report delves into the specific types of care that are often denied, including crucial treatments, medications, and even basic medical services. It also sheds light on the struggles faced by individuals who have been denied access to needed care, highlighting the potential for serious health consequences.
Medicare Advantage Plan Denials: Medicare Advantage Plans Often Deny Needed Care Federal Report Finds

A recent federal report has shed light on a concerning trend: Medicare Advantage plans are increasingly denying needed care to their enrollees. This report highlights a growing problem that impacts the health and well-being of millions of Americans who rely on these plans for their healthcare.
The latest report on Medicare Advantage plans is a stark reminder that the system isn’t always working as it should. It’s not just about the money, though, it’s about people’s health and well-being. This makes me think of the article, forget the great resignation bring on the great reimagination , which argues that we need a fundamental shift in how we think about work and life.
Maybe we need a similar shift in how we approach healthcare, too. We can’t just accept a system that denies needed care; we need to reimagine a system that truly puts people first.
Types of Care Frequently Denied
Medicare Advantage plans are often criticized for denying access to essential medical services, particularly in areas like mental health, physical therapy, and specialty care.
- Mental Health Services:Many enrollees report difficulty obtaining authorization for mental health services, including therapy, medication, and inpatient treatment. The report found that mental health services are often subject to strict pre-authorization requirements and limited network access, making it challenging for individuals to receive the care they need.
- Physical Therapy:Similar to mental health services, physical therapy is another area where Medicare Advantage plans frequently deny coverage. This can pose a significant barrier for individuals recovering from injuries or chronic conditions who require physical therapy to regain mobility and improve their quality of life.
- Specialty Care:Accessing specialists like cardiologists, oncologists, and neurologists can be particularly difficult for Medicare Advantage enrollees. These plans often impose strict referral requirements and limit network access, making it challenging for individuals to see the specialists they need for proper diagnosis and treatment.
Examples of Individuals Facing Challenges
The report includes numerous examples of individuals who have faced significant challenges accessing needed care through Medicare Advantage plans.
- -*Ms. Smith, a 72-year-old woman with chronic back pain, was denied authorization for physical therapy by her Medicare Advantage plan. Her doctor recommended physical therapy as a crucial component of her treatment plan, but the plan refused to cover the costs, citing “lack of medical necessity.” As a result, Ms.
Smith’s pain persisted, and her ability to maintain her daily activities was severely compromised.
- -*Mr. Jones, a 68-year-old man struggling with depression, was denied coverage for a mental health medication by his Medicare Advantage plan. Despite his doctor’s recommendation, the plan required Mr. Jones to undergo a lengthy and bureaucratic prior authorization process before approving the medication.
The delay in accessing his medication significantly impacted his mental health and well-being.
Impact on Beneficiaries
Medicare Advantage plan denials can have a significant impact on beneficiaries, both physically and financially. When individuals are denied access to needed care, it can lead to delays in diagnosis and treatment, worsening health conditions, and increased healthcare costs.
Challenges in Navigating the Appeals Process
The appeals process for denied care can be complex and challenging for beneficiaries. It often involves navigating bureaucratic procedures, gathering supporting documentation, and communicating with insurance companies.
- Many beneficiaries lack the time, resources, or knowledge to effectively navigate the appeals process.
- The process can be lengthy and stressful, adding to the burden of dealing with a health issue.
- Beneficiaries may not be aware of their rights or the options available to them.
Potential Consequences of Delayed or Denied Care
Delayed or denied care can have serious consequences for beneficiaries’ health outcomes.
- Conditions may worsen, leading to increased hospitalization, emergency room visits, and long-term disability.
- Individuals may experience unnecessary pain and suffering, impacting their quality of life.
- The lack of timely access to care can also contribute to higher healthcare costs in the long run.
Regulatory and Policy Considerations
The current regulatory framework governing Medicare Advantage plans and their care denial practices is complex and has been the subject of much scrutiny. The Centers for Medicare and Medicaid Services (CMS) oversees these plans, setting standards for their operations and performance.
It’s crazy to think about how much the world has changed. We’re now talking about Medicare Advantage plans denying care, and how the queen of the clubs, Paris Hilton, has become the queen of the metaverse, as seen in this recent article.
I guess it just goes to show that things are constantly evolving, even when it comes to healthcare and celebrity culture.
However, critics argue that the current regulations are insufficient in protecting beneficiaries from unfair denials of care.
Current Regulatory Framework
The Medicare Advantage program operates under a complex set of regulations, designed to ensure quality care and cost-effectiveness. The regulatory framework encompasses various aspects, including:
- Plan Oversight:CMS is responsible for overseeing Medicare Advantage plans, including their enrollment, operations, and performance. This involves reviewing their network adequacy, provider credentialing, and claims processing.
- Benefit Standards:CMS establishes minimum benefit standards that Medicare Advantage plans must adhere to. These standards ensure that beneficiaries receive essential health services, including preventive care, hospitalization, and prescription drugs.
- Quality Measures:CMS tracks and reports on the quality of care provided by Medicare Advantage plans. This includes measures for patient satisfaction, health outcomes, and adherence to clinical guidelines.
- Appeals Process:Beneficiaries have the right to appeal denials of care. This process allows them to challenge decisions made by their plan and seek a review by CMS or an independent entity.
Potential Policy Changes
Several policy changes could address the issue of care denials in Medicare Advantage plans. These include:
- Enhanced Oversight and Enforcement:Increasing CMS’s oversight and enforcement of plan practices could help prevent unfair denials. This could involve stricter penalties for plans that engage in inappropriate denial practices and more frequent audits to ensure compliance with regulations.
- Transparency and Data Reporting:Requiring plans to provide more transparent data on their care denial rates and practices could empower beneficiaries and policymakers to identify problematic trends. This data could include information on the reasons for denials, the types of services denied, and the outcomes of appeals.
- Standardized Appeals Process:Establishing a more standardized and streamlined appeals process could make it easier for beneficiaries to challenge denials and ensure fair and timely resolution. This could involve simplifying the appeals process, reducing the timeframes for appeals, and providing greater support to beneficiaries navigating the appeals process.
It’s heartbreaking to read about Medicare Advantage plans denying needed care, especially when we see stories like this one where a stranger’s simple act of kindness makes such a huge difference. It’s a stark reminder that while some systems fail, human compassion can still shine through.
We need to advocate for better healthcare access for all, especially for those who rely on Medicare Advantage plans.
- Independent Review of Denials:Creating an independent mechanism for reviewing denials of care could enhance accountability and ensure that decisions are made based on clinical evidence and not financial considerations. This could involve establishing a dedicated agency or task force to review denials and make recommendations to CMS or plans.
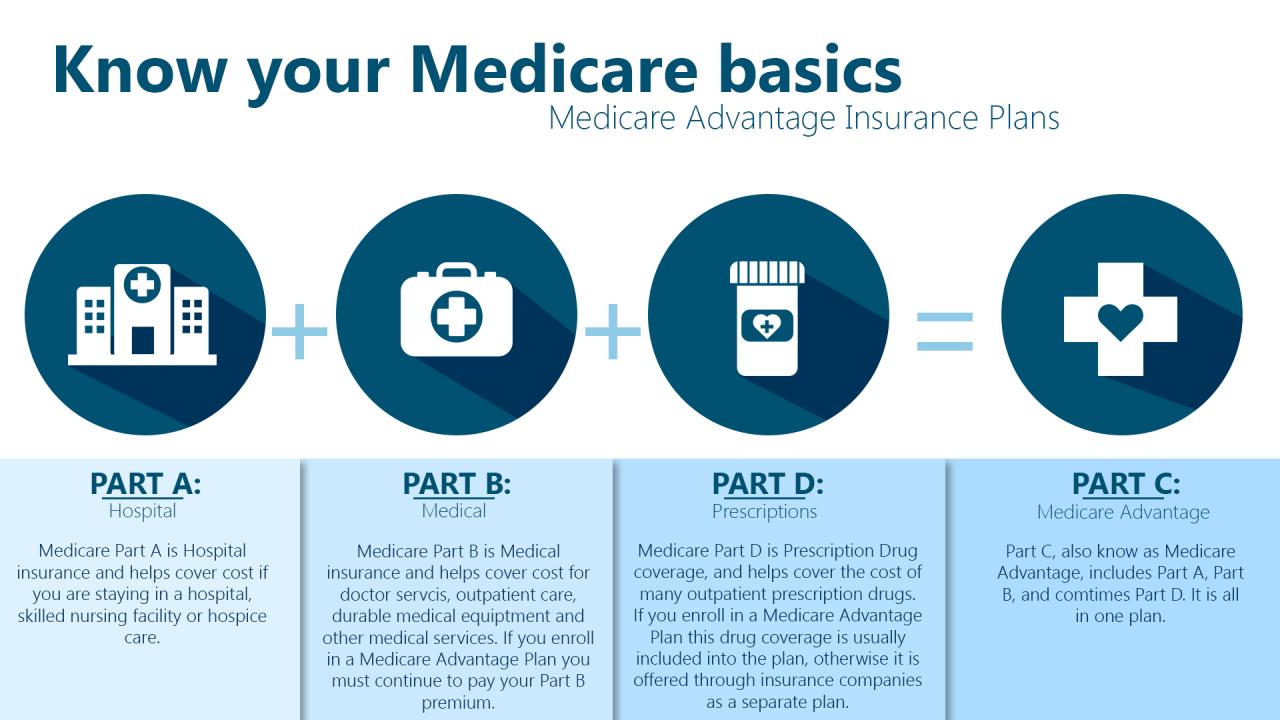
Comparison with Traditional Medicare, Medicare advantage plans often deny needed care federal report finds
While Medicare Advantage plans offer some advantages, such as lower monthly premiums and additional benefits, they also have limitations, including potential restrictions on access to care. Compared to traditional Medicare, Medicare Advantage plans have been shown to have higher rates of care denials, particularly for certain types of services, such as specialty care and mental health services.
- Network Restrictions:Medicare Advantage plans often have narrower provider networks than traditional Medicare, which can limit beneficiaries’ access to certain specialists or facilities. This can lead to denials of care if a beneficiary needs to see a provider outside of their plan’s network.
- Prior Authorization Requirements:Medicare Advantage plans often require prior authorization for certain services, which can delay or deny access to care. This process can be burdensome for beneficiaries and can lead to delays in receiving necessary treatment.
- Utilization Management Practices:Medicare Advantage plans use various utilization management practices, such as step therapy and formulary restrictions, to control costs. These practices can sometimes result in denials of care if a beneficiary’s preferred treatment is not approved.
Provider Perspectives

The challenges faced by healthcare providers in caring for Medicare Advantage beneficiaries are multifaceted and often stem from the complex nature of these plans. The impact of care denials extends beyond financial implications, influencing the provider-patient relationship and access to care for beneficiaries.
Impact of Care Denials on Provider-Patient Relationships
Care denials can significantly strain the relationship between providers and their Medicare Advantage patients. When a provider’s recommended treatment is denied, it can lead to frustration and confusion for both the patient and the provider. Patients may feel abandoned or unheard, leading to a loss of trust in their provider.
Providers, on the other hand, may feel powerless to advocate for their patients’ needs, leading to a sense of professional frustration and a decline in morale.
Financial Implications of Care Denials for Healthcare Providers
Care denials can also have a significant financial impact on healthcare providers. When a treatment is denied, the provider is not reimbursed for the services rendered. This can lead to financial losses for the provider, especially if the denied treatment is complex or requires extensive follow-up care.
In some cases, providers may even be forced to reduce services or staff due to financial constraints.
Public Awareness and Advocacy
Medicare Advantage plans are becoming increasingly popular, but many beneficiaries are unaware of the potential pitfalls associated with these plans. This can lead to denials of care, leaving individuals facing financial burdens and health risks. Public awareness campaigns are crucial to empowering beneficiaries to understand their rights and navigate the complexities of these plans.
Public Awareness Campaign Design
A comprehensive public awareness campaign should aim to educate beneficiaries about their rights and options regarding care denials. Here’s a possible approach:
- Targeted Outreach:Utilize various communication channels to reach different beneficiary segments. This includes senior centers, community organizations, faith-based groups, and online platforms frequented by older adults.
- Clear and Concise Messaging:Develop simple, easy-to-understand materials explaining the basics of Medicare Advantage plans, potential limitations, and the appeals process. Use plain language and avoid technical jargon.
- Real-Life Stories:Share personal stories from beneficiaries who have faced denials and how they successfully appealed them. This adds a human touch and makes the information relatable.
- Interactive Workshops:Organize workshops and seminars led by healthcare professionals and consumer advocates to provide in-depth information and answer questions.
- Partnerships:Collaborate with organizations that work with seniors, such as AARP, to expand outreach and amplify the message.
Medicare Plan Comparison Table
Providing beneficiaries with a clear comparison of different Medicare plans is essential for informed decision-making. The following table highlights key features of Original Medicare and Medicare Advantage plans:
| Feature | Original Medicare | Medicare Advantage |
|---|---|---|
| Coverage | Hospital insurance (Part A) and medical insurance (Part B) | Private health insurance plans that offer benefits similar to Original Medicare |
| Premiums | Standard monthly premiums for Part B, with potential additional premiums for Part A | Vary depending on the plan and location |
| Out-of-Pocket Costs | Deductibles and coinsurance for both Part A and Part B | May have lower deductibles and coinsurance, but often have higher out-of-pocket maximums |
| Network | Nationwide network of providers | Limited network of providers, typically within a specific geographic area |
| Benefits | Covers a wide range of services, including hospitalization, doctor visits, and preventive care | May offer additional benefits, such as vision, dental, or hearing coverage |
| Flexibility | Can see any provider who accepts Medicare | Must stay within the plan’s network |
Resource Guide for Beneficiaries
A comprehensive resource guide should equip beneficiaries with the tools to navigate the appeals process and access other relevant resources.
- Appeals Process:Explain the different levels of appeal, timeframes, and documentation requirements. Include contact information for the Medicare Appeals Council and other relevant entities.
- Consumer Protection Agencies:List contact information for organizations like the Centers for Medicare & Medicaid Services (CMS) and the Medicare Rights Center, which provide guidance and support to beneficiaries.
- Legal Assistance:Highlight legal aid organizations that offer free or low-cost legal representation to beneficiaries facing denials.
- Online Resources:Provide links to websites with comprehensive information about Medicare Advantage plans, appeals procedures, and consumer rights.
- Local Support Groups:Identify local support groups where beneficiaries can connect with others facing similar challenges and share experiences.
Closing Summary
The report’s findings underscore the importance of understanding the complexities of Medicare Advantage plans and the potential risks associated with these programs. It is crucial for beneficiaries to be aware of their rights and options when it comes to accessing healthcare, and to advocate for themselves when faced with denials.
This report serves as a wake-up call, prompting a renewed focus on ensuring that all Americans have access to the care they need, regardless of their insurance plan.

